Head and neck cancer
WHAT IS CANCER?
Cancer is the abnormal growth of a certain type of cell. The cancer can develop locally (in its primary site) or it can spread to other parts of the body, known as metastasis.
Most head and neck cancers are associated with the significant intake of alcohol and/or tobacco products.
What are the symptoms of head and neck cancer?
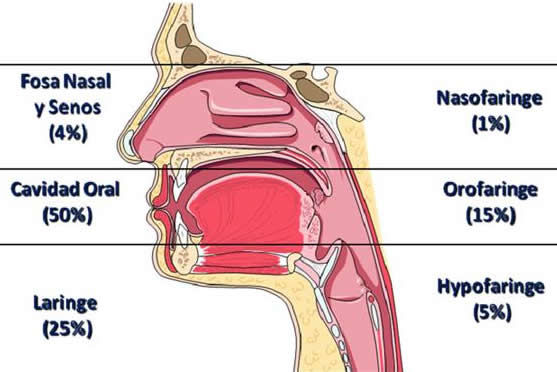
The symptoms will depend on the area where the cancer develops:
- a) In the voice box (larynx) and the throat (pharynx) symptoms include:
- changes to the voice (dysphonia). Patients who smoke should see an ENT specialist (otolaryngologist) if the changes persist after 2 weeks as this could indicate injury to the vocal cords, which are located in the larynx.
- difficulty swallowing (dysphagia)
- blood in the saliva
- pain or irritation in the neck and/or one of the ears
- appearance of a lump on any part of the neck
- only in cases where the cancer is advanced, difficulty in breathing (dyspnoea).
- b) In the nose, sinuses, back of throat behind the nose (nasopharynx) symptoms can include:
- nasal obstruction
- changes to the sound of the voice
- blood coming from the nose, mixed with nasal mucus
- sensation that the ear is blocked
- c) In the mouth, tongue, tonsils and palate the symptoms can include:
- a white or red mark on any part of the mouth
- a lump on the lips, the mouth or the neck, below the jaw
- difficulty swallowing and/or chewing
- an ulcer in any part of the mouth. Patients who smoke and/or drink alcohol, or those who wear a prosthesis in their mouth which causes rubbing, should see an ENT (ear, nose and throat) specialist if the ulcer does not heal after 2 weeks, irrespective of whether it is painful or not.
How is it diagnosed?
ENT specialists (otolaryngologists) use a range of screening techniques that work in combination with each other to diagnose head and neck cancer.
- A fibrolaryngoscopy is performed at our clinic and takes a few seconds;
- Radiological screening: CAT (computerised axial tomography), MRI (magnetic resonance imaging) and PET (positron emission tomography) scans;
- FNA (fine-needle aspiration): a technique involving the insertion of a fine needle into the affected tissue. It is completely painless, is performed at our clinic and allows cells to be collected for examination with a microscope;
- Biopsy of the affected tissue in order to analyse the cells and confirm whether or not they are cancerous.
How is it treated?
The treatment of head and neck cancer will
depend on the location of the tumour, its size and whether or not it has spread (metastasis), either to other organs (lung, bones) or to the surrounding lymph nodes.
By using a combination of exploration techniques, radiological screening and biopsy, we will obtain enough information to determine the right treatment for the head and neck cancer.
Treatments for head and neck cancer, both single and combination, include:
- Surgery to completely remove the tumour. In most cases, this is performed with the CO2 laser, which allows us to remove all of the tumour, with minimal bleeding and no pain. Another benefit of laser surgery is that it avoids unnecessary scars, the need for a tracheotomy (making a small hole in the neck) and swallowing difficulties;
- If the cancer spreads to the surrounding lymph nodes in the neck, they will also be removed together with the tumour;
- Radiotherapy involves the use of high-energy radiation to kill the cancerous cells. It can be a single treatment, used in combination with chemotherapy, or in addition to surgery to remove microscopic traces of the disease;
- Chemotherapy involves the use of medication to kill the cancerous cells. It can be administered orally, or via an intravenous or intramuscular injection. Chemotherapy can be a single treatment or a treatment in combination with surgery and/or radiotherapy.
×Nuestro sitio web usa cookies para mejorar la experiencia de usuario, conocer sus hábitos de navegación y ofrecerle mejor contenido.
Si continúa navegando por el sitio entendemos que da su consentimiento a nuestra política de cookies. Aceptar
Our website uses cookies in order to improve your user experience, know your navigation habits and offer you better contents.
By using this website you consent to our cookie policy. Accept
Our website uses cookies in order to improve your user experience, know your navigation habits and offer you better contents.
By using this website you consent to our cookie policy. Accept
Our website uses cookies in order to improve your user experience, know your navigation habits and offer you better contents.
By using this website you consent to our cookie policy. Accept
El nostre lloc web fa servir cookies per millorar l'experiència d'usuari, conèixer els seus hàbits de navegació i oferir-millor contingut.
Si continua navegant pel lloc entenem que dóna el seu consentiment a la nostra política de cookies. D'acord

 by Develona
by Develona